- Home
- About
- Education
- Upcoming SGS Meetings
- Patient Resources
- Past Scientific Programs and Abstracts
- Past Social Media Committee Workshop Presentations
- 2023 Social Media Committee Workshop Presentation
- 2022 Social Media Committee Workshop Presentation
- 2021 Social Media Committee Workshop Presentation
- 2019 Social Media Committee Workshop Presentation
- 2018 Social Media Committee Workshop Presentations
- 2017 Social Media Committee Workshop Presentations
- 2016 Social Media Committee Workshop Presentations
- Simulation Advisory Service
- Video Library
- Webinars
- Research
- Membership
- Mentorship
- Donate
- Events
- Contact
 Joint Statement on Re-introduction of Hospital and Office-based Procedures in the COVID-19 Climate for the Practicing Gynecologist Traditionally, surgical procedure prioritization depends on illness acuity and resource availability after shared decision making with patients. During an emergency such as the COVID-19 pandemic, decisions must take into consideration new influences on the safety of benign gynecologic procedures. Prioritization of patients must be fluid as the pandemic waxes and wanes and is likely different in the peaks than the troughs of infection incidence. At the peak of the infectious curve, all surgeries except those that are a threat to life or limb are cancelled, as the risk to individuals coming out of self-isolation is high and could overwhelm already taxed health care resources. The trough represents a new normal, where the risk of COVID-19 infection still remains, but at a diminishing rate. In the trough, the risk of infection to individuals scheduled for surgery must be weighed against the morbidity of their benign condition. In this scenario, patients with severe comorbidities, or those who would require rehabilitation or a skilled nursing facility after surgery should consider delaying surgery until a vaccine or effective therapy is available. Between peak and trough, the decision to proceed with surgery lies in between the two extremes. In the deceleration phase, liberalizing restrictions should start with individuals with urgent conditions who are severely affected by their gynecologic condition, weighed against their underlying health condition. How to prioritize surgeries, weighed against the risk to patients of undergoing surgery during a pandemic, has necessitated the development of tiered systems that can adapt to quickly changing environments.
The American College of Surgeons (ACS) developed several tiered ranking systems for prioritization of surgeries. (1,2) The first scale outlines how an institution should prioritize staffing and utilization of resources and ranges from “Alert” to “Condition Zero” based on the number of patients with COVID-19 who are admitted to the hospital. The second scale is the “Elective Surgery Acuity Scale”. This is a tiered scale ranging from 1-3; the first tier are elective surgeries, the middle tier are urgent surgeries, and the third tier are emergency surgeries. Each tier is further dichotomized into patients with and without significant comorbidities. Similar to the ACS tiered response, Goldman et al, described a tiered system ranging from “0”, emergency surgeries and outpatient procedures that should be performed at the peak of the curve to “4”, non-essential surgeries that can be delayed until the threat of infection has subsided for urologic procedures.(3) In addition, there has been a publication by Weber LeBrun et al. that outlines the initial response to the COVID pandemic, but does not follow the ACS tier system.(4)
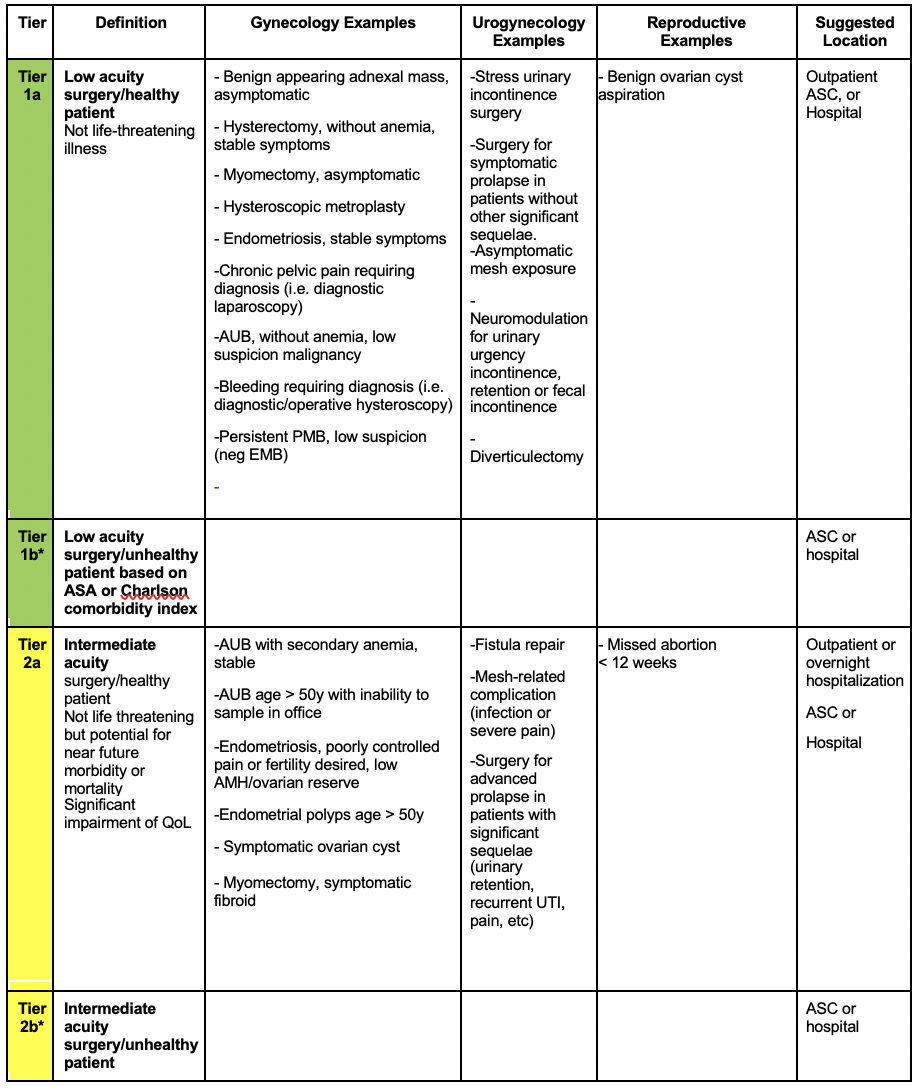
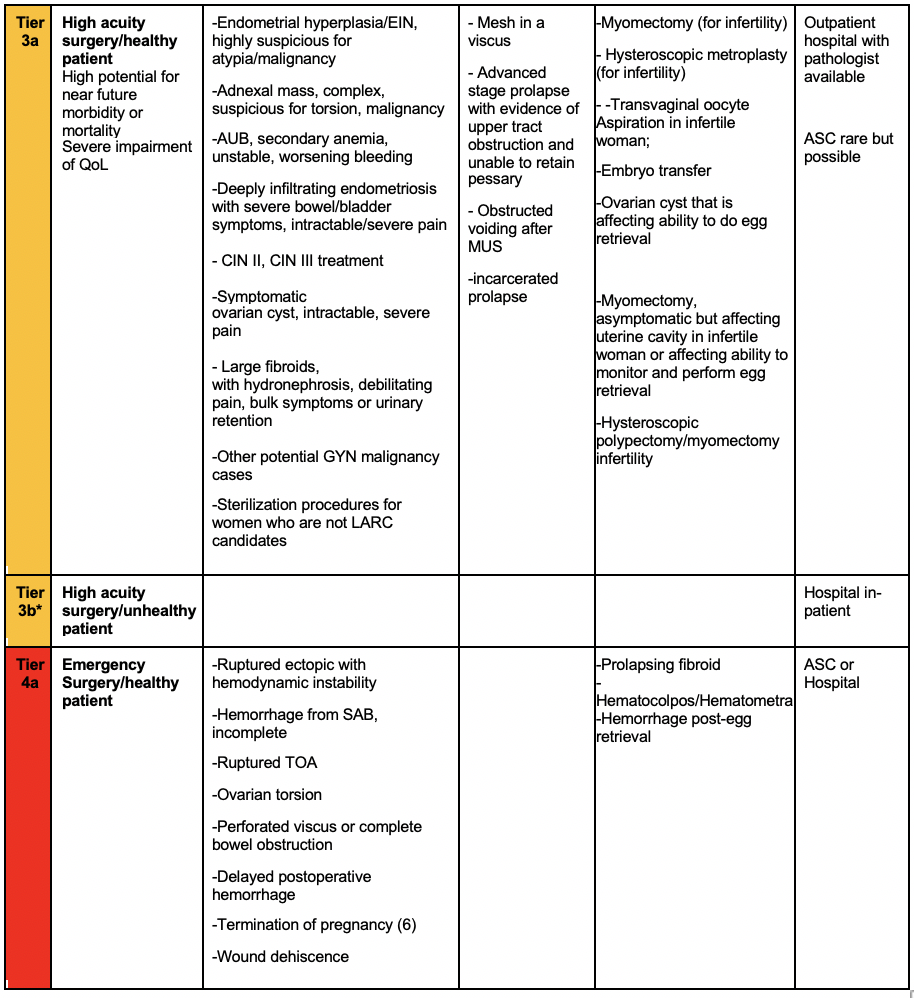
We have adapted the ACS tiered ranking list to develop guidance for general gynecologic, urogynecologic, and reproductive surgeons. (Figure 1) The system is meant to help surgeons and their health care systems decide who should go to the operating room as the pandemic unfolds and does not list all elective surgeries in each tier. This guidance is not meant as a substitute for clinical judgement of an individual surgeon and the process of shared decision making with patients. This is particularly important for women with medical comorbidities in whom increased exposure to infected individuals outside the home outweighs the urgency of their gynecologic condition. Continued use of telemedicine to address symptom management while surgery is delayed may be helpful.
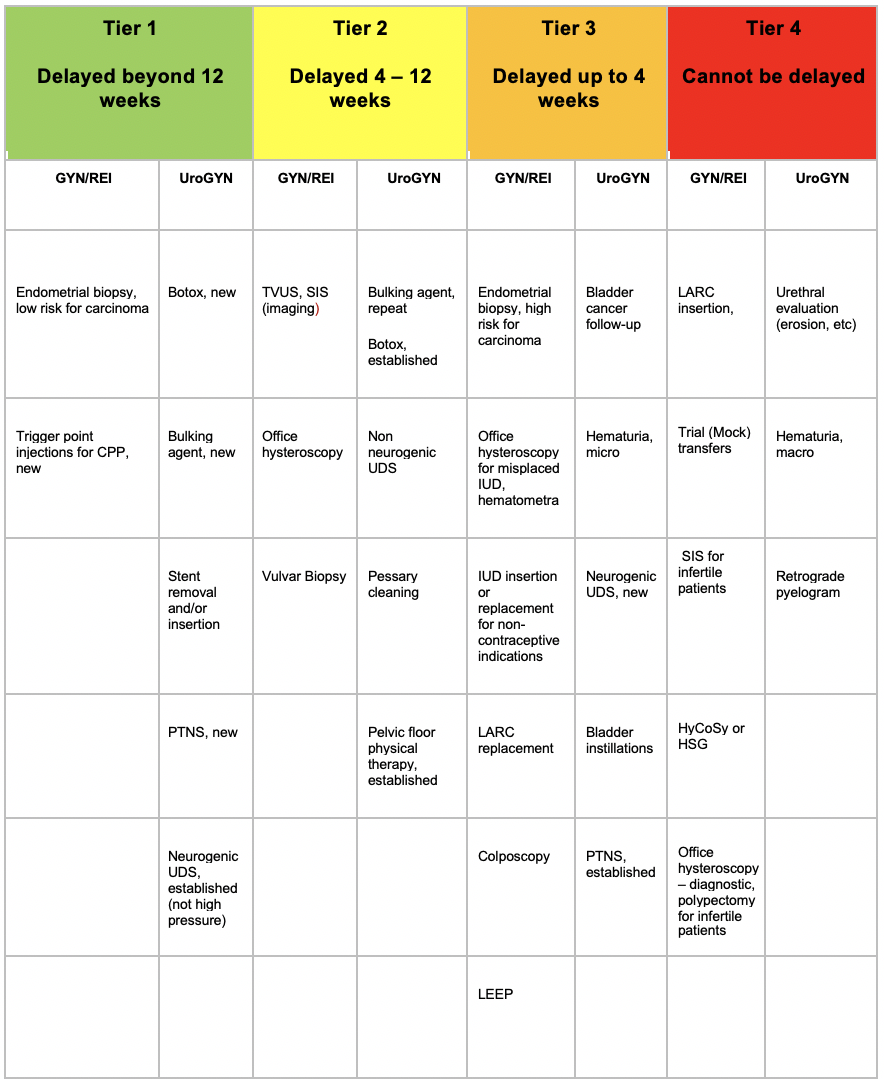
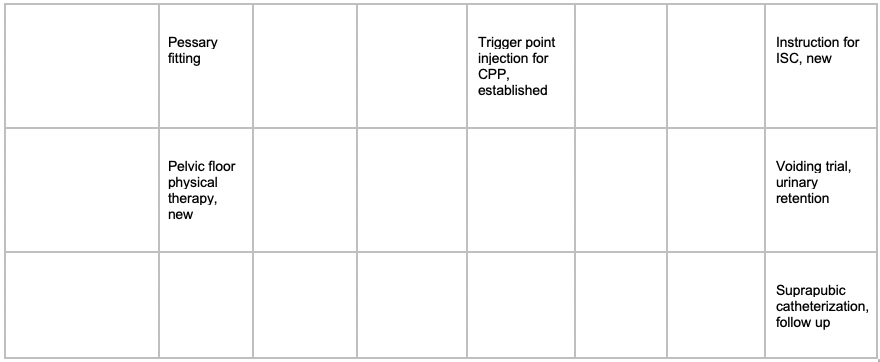
In addition, we have applied the tiered system to office-based procedures. (Figure 2) All decisions should be made in the context of local and state directives. Many places across the globe have been in the “Condition Zero” level of planning where all but emergency surgeries are cancelled, regardless of the prevalence of COVID-19 cases in a specific area. As we approach reopening surgical services to women with non-emergent surgical problems, a new calculus is needed. The tiered system must take into account the patient’s gynecologic condition, as well as their medical comorbidities, and be able to adapt to changing conditions, as we re-open, and re-close, gynecologic surgery services for women through the pandemic. Surgical technique and personal protective equipment availability must also be considered.(5) Local disease prevalence and reopening strategies may supersede this document and we defer to clinical decision making in coordination with other local resource considerations. Figure 1: Modified Elective Surgery Acuity Scale (mESAS) for Benign Gynecologic Indications and Surgeries
*Tier “b” indicates patients with complicated medical conditions that, in the environment of COVID-19, may place them at high risk for ICU admission and increased perioperative morbidity and mortality. This will likely affect the order of prioritization of individuals for surgery. For example, in an environment where we are just opening surgical suites, we may determine that even though the acuity of the surgical problem is high, that the tier 3b women would not go to surgery prior to the tier 2a women. On the other hand, when the risk of COVID morbidity and mortality is lower, a tier 3b woman might go ahead of tier 2a woman who is healthy. Ranking of the tiers is dependent on the COVID environment. AMH: anti-mullerian hormone; ASC: ambulatory surgery center; AUB : abnormal uterine bleeding; CPP Chronic pelvic pain; EIN: endometrial intra-epithelial neoplasm; LARC: long-acting reversible contraception; MUS: mid-urethral sling; SIS: saline infusion sonography; SAB: spontaneous abortion; TOA: tubo-ovarian abscess; TVUS: transvaginal ultrasonography; PMB: postmenopausal bleeding; UDS: urodynamics; EMB: Endometrial biopsy; UTI: urinary tract infection
CPP: Chronic pelvic pain; ISC: intermittent self-catheterization; IUD: intra-uterine device; LARC: Long-acting, reversible contraception; LEEP: Loop electrosurgery excision procedure; PTNS: percutaneous tibial nerve stimulation; SIS: saline infusion sonography; TVUS: transvaginal ultrasonography; UDS: urodynamics; HyCoSy; Hysterosalpingo contrast sonography: HSG; hysterosalpingogram References:
|